Why Your Medication Might Not Be Working the Way You Intended
Reviewed by Ashley Robinson, PharmD, Pharmacy Manager for TelyRx

Table of Contents
You got your new prescription, read the label twice, and took it exactly as directed. But now, a week or two in, it doesn’t seem to be working. Maybe the relief you expected hasn’t kicked in. You might even be wondering if what you’re taking is the real thing.
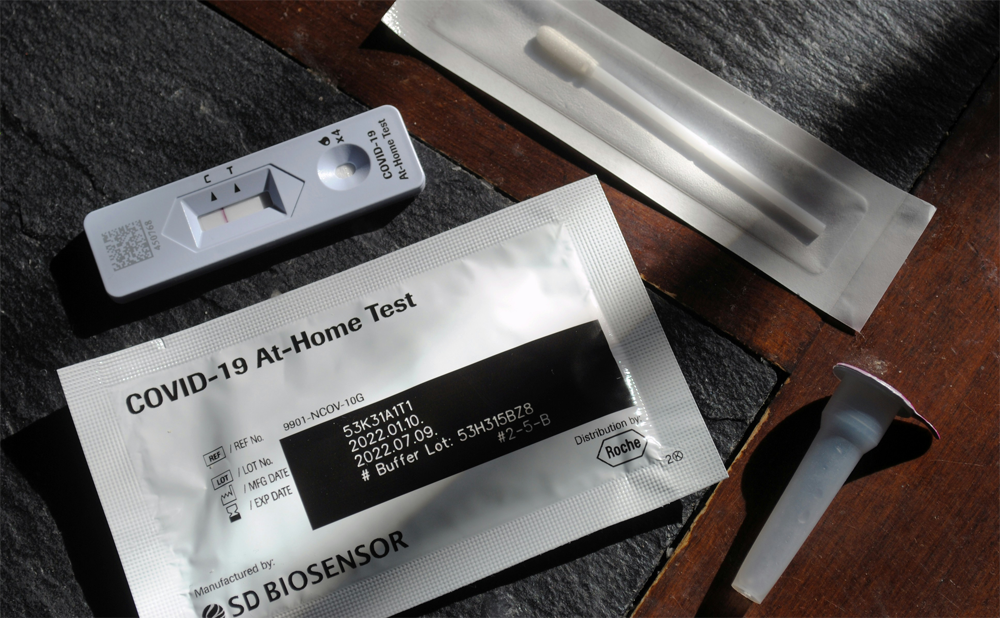
Before you jump to conclusions or assume you’ve received a defective or counterfeit product, let’s talk about what’s actually happening. First, the U.S. drug supply is among the safest in the world, with federal and state laws creating a ‘closed’ drug distribution system to help ensure medications are safe.
When you get medication from a state-licensed pharmacy—whether online or in-person—variations in the way it works or feels are usually about your body’s response, not the medication’s authenticity. Each person’s response to medication is complicated, highly personal, and influenced by far more factors than just the pill itself.
does online medication work the same?
Here’s a question that comes up a lot: if you ordered your medication online, is it the same as what you’d get at a brick-and-mortar pharmacy, like a CVS or Walgreens?
The short answer is, yes. It’s exactly the same, provided it was dispensed by a state-licensed pharmacy.
All FDA-approved medications dispensed through licensed pharmacies—including online pharmacy platforms like TelyRx—are sourced from the same FDA-verified suppliers and distributors used by major pharmacy chains. The regulations are identical. The safety standards are identical. The active ingredients are identical. Licensed online pharmacies operate under the same strict federal oversight and quality control as traditional pharmacies.
So, if a medication feels different or less effective than you expected, it’s almost certainly not because you ordered it online. It’s more likely the result of how your particular body is processing it—and this is where things get interesting.
your body isn't a machine
Medications don’t work in isolation. They work inside a human body that is shifting and adapting at every moment.
Your body is constantly changing in ways you might not even notice. Weight fluctuations, hormone shifts, stress levels, sleep quality, hydration, diet—all of these can alter how your body metabolizes medication. For example, your liver enzymes (which break down many medications) can speed up or slow down depending on what else is going on in your system. Your stomach acidity can shift based on what you ate that day, and this can affect how much of the medication actually gets absorbed.
This is especially true for maintenance medications like those for anxiety, blood pressure, or chronic pain. Your body adapts. Your baseline shifts. What worked perfectly six months ago might feel less effective now; not because the medication changed, but because you did.
And sometimes, the changes are temporary. A bad week of sleep, a stressful month at work, or a bout of dehydration can all throw off how well a medication works, even if you’re taking it exactly the same way.
Pharmacogenomic testing can reveal how your body is genetically programmed to process certain types of medications, showing whether you’re a fast, normal, or slow metabolizer of specific drugs. This genetic variation explains why the same dose can work perfectly for one person and do nothing for another.
timing and consistency matter more than you think

Here’s something most people don’t realize: skipping doses or changing the time of day you take your medication can completely alter how well it works.
Some medications—like birth control pills, antihistamines, or blood pressure meds—need steady, consistent levels in your bloodstream to be effective. Miss a day, and those levels drop. Take it at different times, and you’re constantly playing catch-up. Your body never gets the chance to reach that therapeutic sweet spot where the medication can work at its full potential.
And then there’s the food factor. Some medications need to be taken on an empty stomach to absorb properly, while others need to be taken with food to avoid nausea or improve absorption. Food can significantly enhance or reduce the extent of drug absorption, which directly affects how well the medication works.
So, if your medication isn’t working the way you expected, ask yourself: am I taking this the exact same way, at the exact same time, every single day? If the answer is no, that might be your answer.
drug interactions you might not expect

Even if you’re taking your medication perfectly, other things you consume could be altering its effectiveness. Here are some common examples:
- Antacids or calcium supplements can block absorption of thyroid medication and certain antibiotics.
- Grapefruit juice interferes with the metabolism of many medications—including certain blood pressure, cholesterol, and erectile dysfunction drugs—typically making them stronger than intended, which can cause side effects.
- Alcohol can intensify sedative effects and reduce the effectiveness of other medications entirely.
- Caffeine can counteract certain medications or make side effects worse.
And the potential interactions don’t stop there. If you’re taking multiple medications or over-the-counter supplements, these can interact with each other in ways that diminish effectiveness or amplify side effects. Your multivitamin might be harmless on its own, but paired with certain prescriptions, it could cause a problem.
If you feel your medication is not working as effectively as you’d like it to, consider keeping a running list of everything you take—prescription meds, over-the-counter remedies, vitamins, supplements, even herbal teas—and share this with your pharmacist or primary care doctor at every appointment. It’s the easiest way to help them identify potential drug interactions before they cause problems.
generics, brand names, and the formulation shuffle

Let’s talk about generics, because this is where a lot of confusion happens.
Generic medications use the same active ingredients as their brand-name counterparts, with the same dosage and therapeutic effect. The FDA requires this. But here’s the catch: generic versions may include different inactive ingredients such as fillers, binders, and coatings, and these can affect how the medication dissolves or is absorbed in your body.
This doesn’t mean the generic is “weaker” or “fake.” It just means it might feel slightly different. For most people, the difference is negligible. But for some, especially with medications that have a narrow therapeutic window (like thyroid meds or blood thinners), even a small change in absorption can be noticeable.
And here’s something else many people don’t know: even if you’re getting the “same” generic every month, the manufacturer might change. Different pharmacies use different suppliers. Different batches come from different facilities. All of this is within FDA standards, but small variations can happen.
how you store your medication matters
Medications are sensitive. Heat, humidity, and light can degrade their potency over time.
If you’re keeping your pills in a steamy bathroom, on a sunny windowsill, or in a hot car, you might be compromising their effectiveness. This is especially true for liquids, inhalers, and gel capsules, which are more vulnerable to environmental changes.
TelyRx’s licensed pharmacies operate within temperature-controlled facilities to ensure medications arrive at full potency. But once they’re in your hands, proper storage becomes your responsibility. Keep them in a cool, dry place, and not the bathroom medicine cabinet, despite the name.
Also, check expiration dates. Expired medications lose their potency, potentially producing a weaker response, or none at all If your medication isn’t working and it’s been sitting in your cabinet for two years, that might be why.
the medical condition itself may change over time
Here’s the hard truth: sometimes it’s not the medication that’s different. It’s you.
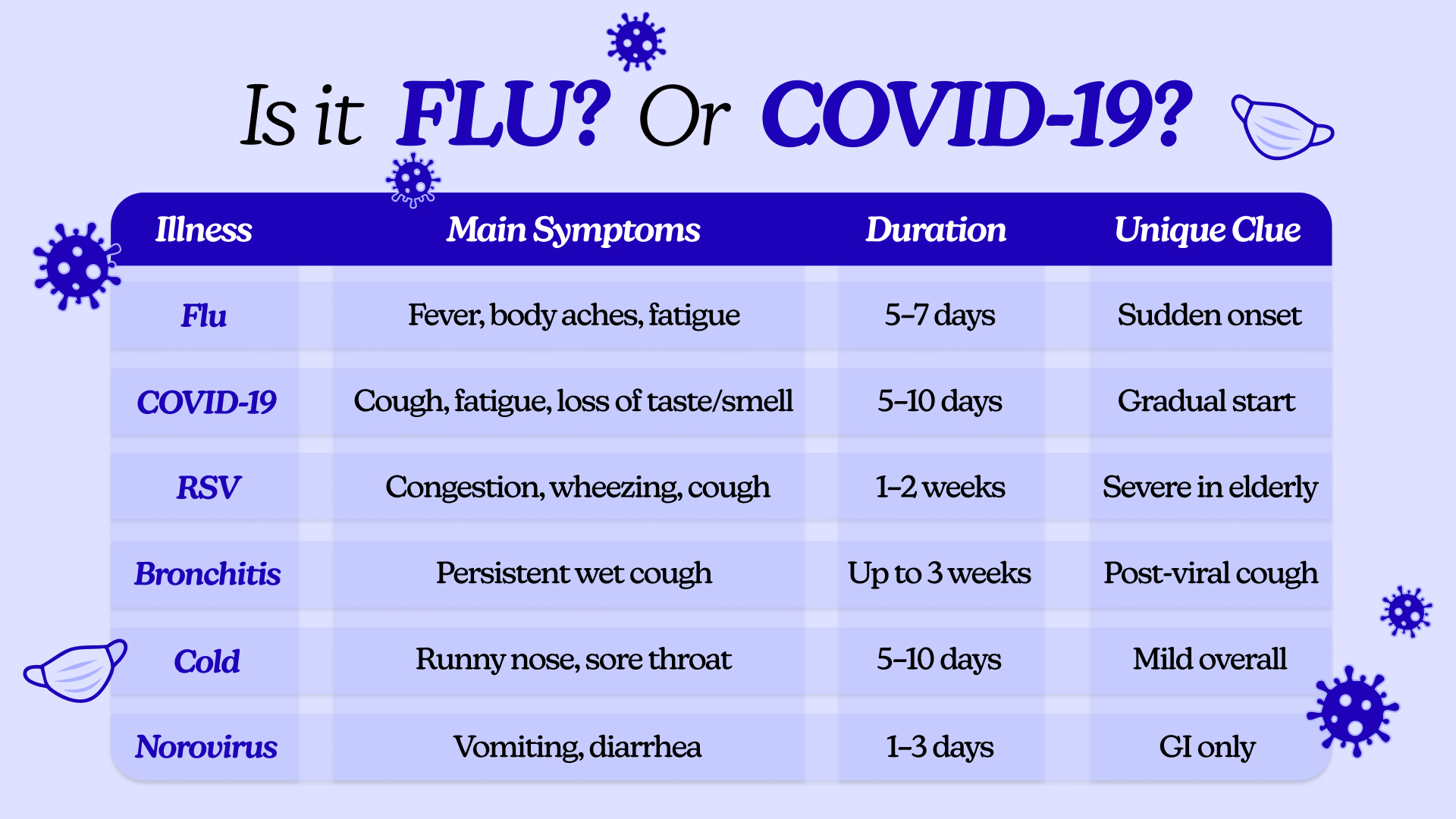
Chronic conditions like migraines, high blood pressure, allergies, or chronic pain don’t stay static. They fluctuate based on stress, weather, illness, hormones, sleep, and dozens of other factors. A medication that worked perfectly three months ago might not be cutting it anymore. This is not because the medication changed, but because your condition did.
This is especially common with conditions affected by lifestyle and environment. Your stress levels shift. Your diet changes. Your body adapts. The dosage that used to control your blood pressure or prevent migraines might not be enough anymore. That doesn’t mean the medication is bad. It just means it’s time to reassess.
If your symptoms are breaking through despite consistent medication use, it might be time to talk to your provider about adjusting your dosage or trying something new.
what to do if you suspect your medication isn't working
If your medication doesn’t seem to be working, you have options. Don’t panic, and definitely don’t stop taking it cold turkey. Here’s what to do instead:
Step 1: Track what’s happening.
Note the following in writing: What time of day do you take your medication? What do you eat and drink before and after? If you’re having breakthrough symptoms or side effects, do you notice any patterns? Having this concrete data makes it a lot easier to figure out what’s going on.
Step 2: Talk to your provider or pharmacist.
Share what you’re experiencing. It might be a dosage issue, an interaction with something else you’re taking, or a sign that you need a different formulation. Your provider can’t help troubleshoot if they don’t know what’s going on.
If you’re working with a platform like TelyRx, you can quickly connect with a licensed pharmacist for helpful guidance without waiting weeks for an appointment.
Step 3: Understand the no-return rule.
You may not realize it, but federal law prohibits pharmacies—online and retail—from accepting returned prescription medications for resale or reuse once they’ve left the pharmacy. This isn’t a company policy. It’s a safety regulation designed to prevent tampering, contamination, or counterfeit drugs from re-entering the supply chain.
medication effectiveness is highly personal
Here’s the bottom line: medication effectiveness isn’t a one-size-fits-all proposition.
Small variations in formulation, timing, food, stress, sleep, and dozens of other factors can make a big difference in how a medication works. That doesn’t mean the medication is fake, unsafe, or ineffective. It just means your body is complex and constantly adapting.
If you’ve been taking your medication consistently for 1–2 weeks and you’re still not seeing results, or if the side effects are outweighing the benefits, it’s time to talk to your provider. Sometimes you need a different formulation, a different dosage, or a completely different drug. That’s not a failure. It’s just part of finding what works for your body.
The best results come from consistency, communication, and collaboration with a provider who listens. If something feels off, don’t ignore it. Track what’s happening, ask questions, and never hesitate to speak up when something doesn’t feel quite right.
Disclaimer
This blog post is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. The content provided here is not a substitute for professional medical advice, consultation, or care from a qualified healthcare provider. Always seek the guidance of your physician or another licensed health professional with any questions you may have regarding a medical condition or treatment. Do not disregard or delay seeking professional medical advice based on information read on this site. Learn more about our editorial standards here.