Surprising Takeaways:
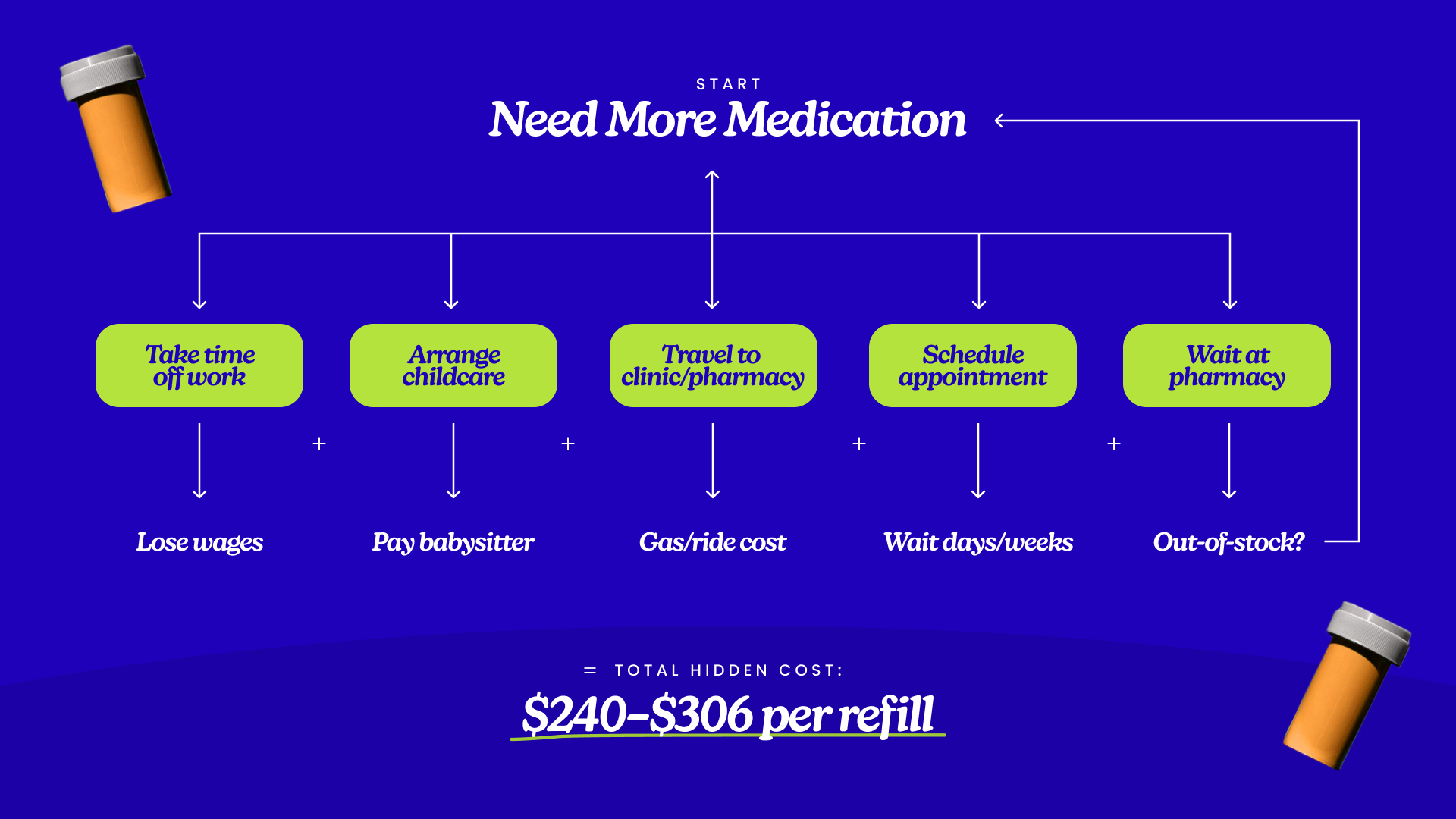
- A “routine” refill can cost $240–$290 once you factor in doctor visits, lost wages, transportation, and childcare — not including the medication itself, time spent seeking your refills, or any emotional/physical stress.
- Patients with quarterly refills can spend over $1,000 a year on hidden costs just to stay on a single medication.
- Prior authorization time averages 3 days, with 31% of patients waiting more than a week before their medication is approved when using insurance.
- Pharmacy closures and national drug shortages often force patients into repeat trips, longer travel, and added delays, with 1 in 3 pharmacies closing between 2010 and 2021.
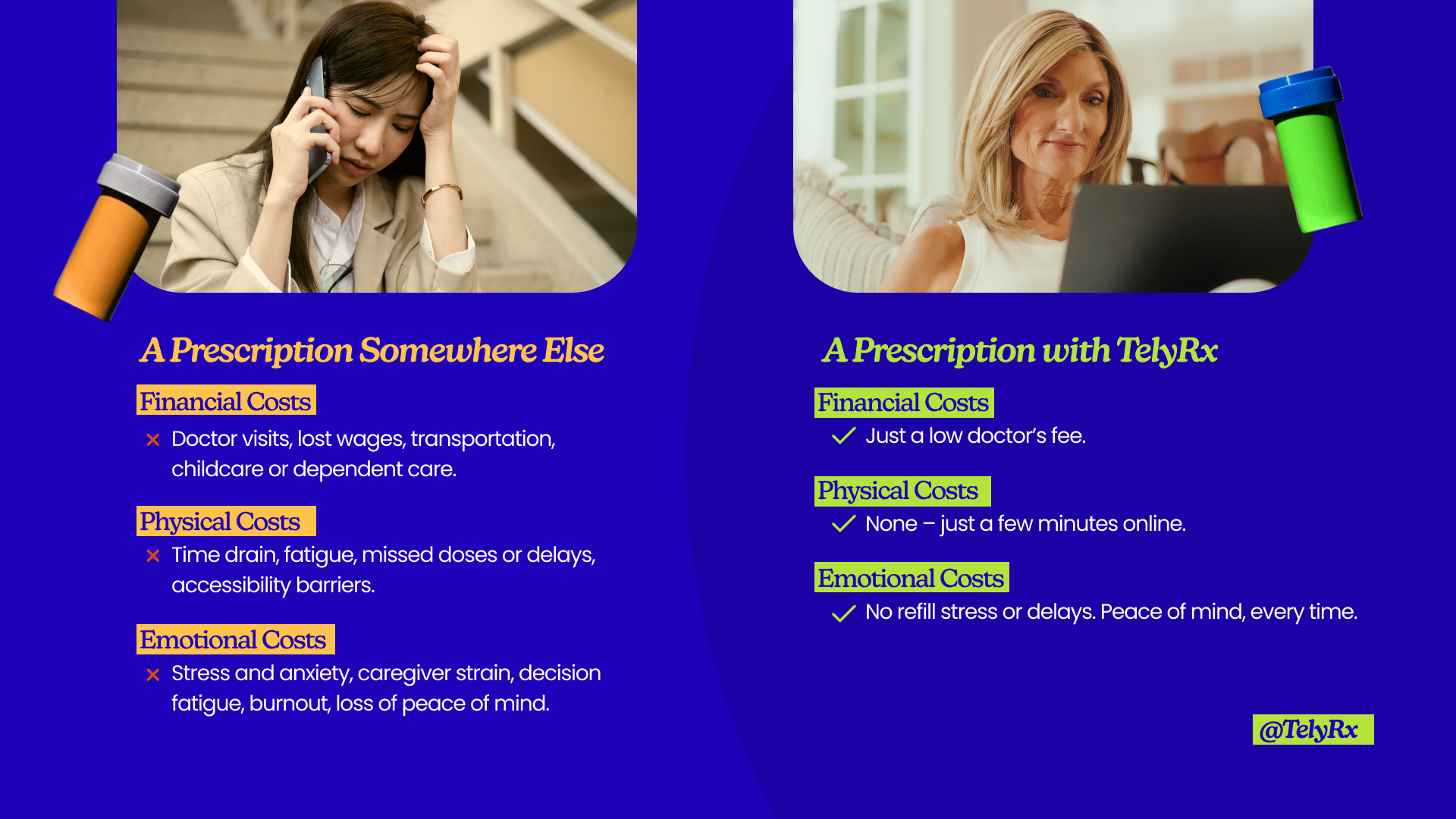
- Beyond money, refills drain patients physically and emotionally: hours wasted in pharmacy lines, the stress of running low, the strain of arranging childcare or dependent care, the fatigue of repeated trips, and constant calls to doctors requesting refills.
- These burdens fall hardest on chronic illness patients, rural residents, working parents, and seniors living alone, turning “routine” care into an exhausting obstacle course.