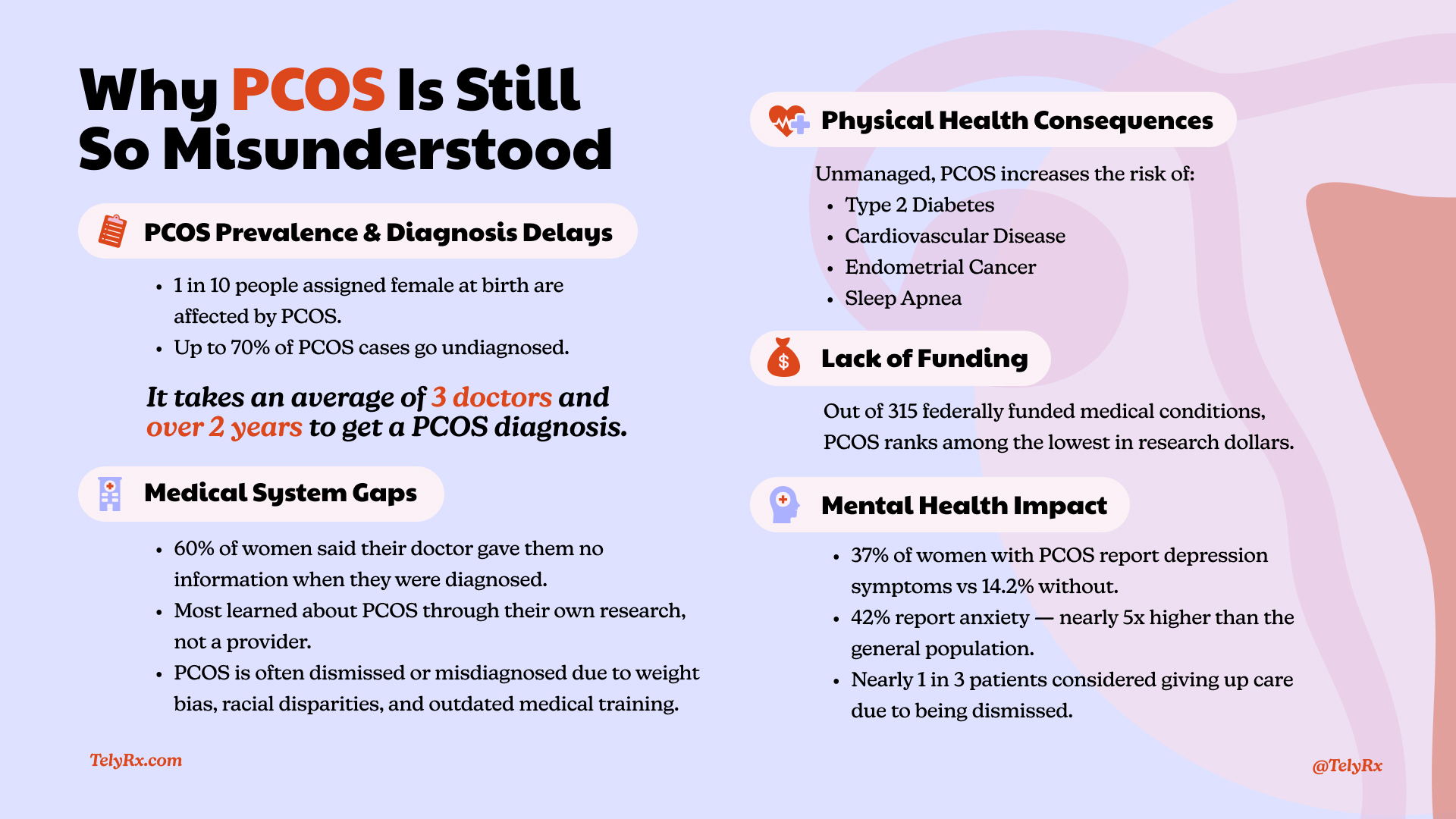
Here’s something that might surprise you: Polycystic Ovary Syndrome (PCOS) affects roughly 1 in 10 people assigned female at birth—that’s an estimated 6–13% of reproductive-aged women.
Yet somehow, countless patients spend years bouncing between doctors, being undiagnosed or misdiagnosed, receiving conflicting information, or being told their symptoms are “just part of being a woman.” Sound familiar?
Even with increased awareness in recent years, PCOS still remains deeply misunderstood — not just among the general public, but within the healthcare system itself. Misconceptions, outdated training, weight bias, and a lack of research funding have all contributed to widespread diagnostic delays and treatment gaps.
Let’s explore the complex nature of PCOS, what a delayed diagnosis actually costs women both emotionally and physically, and how we can all push for the care, validation, and positive outcomes that everyone deserves.